“Researchers from Penn have developed a scalable microfluidics platform that could transform RNA therapeutic and vaccine production.
Following the global COVID-19 pandemic, the development and rapid deployment of mRNA vaccines highlighted the critical role of lipid nanoparticles (LNPs) in the context of pharmaceuticals. Used as the essential delivery vehicles for fragile RNA-based therapies and vaccines, LNPs protect the RNA from degradation and ensure effective delivery within the body.
Despite their critical importance, the large-scale manufacturing of these LNPs saw numerous bottlenecks during the pandemic, underscoring the need for scalable production techniques that could keep pace with global demand.
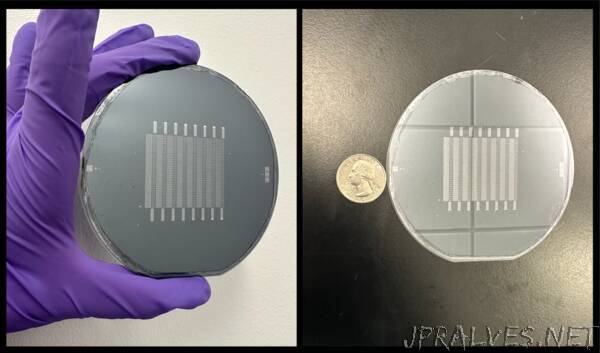
Now, in a paper published in the Proceedings of the National Academy of the Sciences, researchers at the University of Pennsylvania describe how the Silicon Scalable Lipid Nanoparticle Generation platform (SCALAR), a reusable silicon- and glass-based platform designed to transform the production landscape of LNPs for RNA therapeutics and vaccines, offers a scalable and efficient solution to the challenges exposed during the COVID-19 crisis.
“We’re excited to create a piece of technology platform that bridges the gap between small-scale discovery and large-scale manufacturing in the realm of RNA lipid nanoparticle vaccines and therapeutics,” says co-author Michael Mitchell, associate professor of bioengineering in the School of Engineering and Applied Science at Penn. “By doing so, we’ve effectively leapfrogged the clunky, time-consuming, and costly barriers that slow down the production ramp-up of promising new RNA medicines and vaccines.”
The intricacies of RNA-based therapies require the RNA to be encased in a delivery system capable of navigating the body’s biological obstacles. LNPs fulfill this role, allowing the RNA to reach the intended cells for maximum therapeutic impact. SCALAR aims to take this a step further, allowing for an unprecedented three orders of magnitude scalability in LNP production rates, addressing the speed and consistency bottlenecks that hinder existing methods.
Sarah Shepherd, the first author of the paper and a recent Ph.D. graduate who worked in the Mitchell Lab, says, “With SCALAR, we’re not just reacting to today’s challenges but proactively preparing for tomorrow’s opportunities and crises. This technology is flexible, uses mixing architectures well-documented in microfluidics, and is scalable enough to meet future demands in real time. That’s an enormous leap forward for the field.”
Shepherd says that SCALAR builds on prior work from the Mitchell lab and is based on a microfluidic chip platform. Akin to a computer chip, wherein a computer’s electrically integrated circuit has numerous little transistors transporting signals as ones or zeroes to produce an output, the SCALAR microchip precisely controls their two key reagents, lipids and RNA, to generate LNPs.
In addition, their platform can have one, 10, or 256 individual mixing units to correspond to the needs-of-use cases ranging from small-scale drug screening and development, to mid-scale formulations for in vivo studies, to large-scale formulations for clinical applications.
To ensure consistency across scales, the same microfluidic mixing architecture is used for all devices, and, to ensure that the two key reagents are uniformly distributed to each device in the array, the team integrated high fluidic resistance microchannels into the design to follow previously established design rules for large-scale microfluidic devices. This guarantees that each device in the multi-unit array produces LNPs with identical physical characteristics, a key attribute in the tightly regulated pharmaceutical industry.
“We’re thrilled we’ve been able to use the clean room at the Singh Center to fabricate multi-purpose chips that can withstand the high heat and harsh solvents needed to clean the chips, making them safely reusable,” Shepherd says.
The SCALAR chips are made from silicon and glass, which provide several advantages over existing polymer-based platforms. Not only do they prevent material-leaching issues associated with these platforms, which lead to contamination, but they also allow for sterilization at extremely high temperatures, making them ideal for pharmaceutical applications. Furthermore, the platform can be reset and reused, offering environmental benefits and reducing overall manufacturing costs.
While the researchers initially used the SCALAR platform to formulate SARS-CoV-2 spike-encoding mRNA LNP vaccines, they believe that the applications are far broader.
“In addition to solving a current and critical need in the pharmaceutical industry, Sarah’s work is a virtuosic combination of microfabrication, microfluidic, and lipid nanoparticle technologies,” says coauthor David Issadore, professor of bioengineering in the School of Engineering and Applied Science at Penn. “There are very few students who could have pulled off something this ambitious in the timeline of a Ph.D.”
“This technology has the potential to become a cornerstone in the field of nanomedicine, beyond RNA-based therapies,” Mitchell says. “The scalability and adaptability of the SCALAR chips could well make them the Swiss Army knife in the RNA lipid nanoparticle pharmaceutical manufacturing tool kit.”
Michael Mitchell is an associate professor in the Department of Bioengineering in the School of Engineering and Applied Science and the director of the Lipid Nanoparticle Synthesis Core at the Penn Institute for RNA Innovation at the University of Pennsylvania.
David Issadore is a professor in the Department of Bioengineering and Electrical and Systems Engineering in the School of Engineering and Applied Science at Penn.
Sarah J. Shepherd is a recent Ph.D. graduate of Penn’s School of Engineering and Applied Science and worked in the Mitchell Lab.
Other authors of the paper are Xuexiang Han, Alvin J. Mukalel, Rakan El-Mayta, Ajay S. Thatte, Marshall S. Padilla, and Daeyeon Lee of Penn’s School of Engineering and Applied Science and Mohamad-Gabriel Alameh, Neha Srikumar, and Drew Weissman of the Perelman School of Medicine at Penn.
This work was supported by the National Science Foundation (Grant NNCI-2025608 and Award 1845298), National Institute of Health (Grants DP2 TR002776, NCI R01 CA241661, NCI R37 CA244911, NIDDK R01 DK123049, 5R21CA236653, 5RM1HG010023, R01HL160616, and T90DE030854), and Burroughs Wellcome Fund.”
